Breasts play a crucial role in a woman’s physiological and psychological well-being, serving as a symbol of femininity. The concept of breast beauty varies for each individual, as every human body is unique. For women with tuberous breasts, aesthetic breast surgery offers an excellent opportunity to correct these malformations, resulting in harmonious, balanced, and desirable breasts without visible after-effects or physiological consequences.

Breast size and shape differ among women, reflecting the vast diversity of human morphology. While tuberous breasts do not affect the primary physiological function of breastfeeding or breast sensitivity, they are considered a breast ‘malformation’. Unlike breast ptosis, tuberous breasts result from a growth deficiency in the lower and median parts of the mammary gland. This condition is less severe than Grade III invaginated (or inverted) nipples, which can interfere with breastfeeding. However, it can cause significant distress to affected teenagers and women, particularly when the breasts are asymmetrical.
Although pronounced tuberous breast syndrome affects only one in 2000 women, specialists believe that tuberous breasts could affect at least 10% of women due to frequent underdiagnosis. Minor to moderate cases may not prompt women to seek medical advice, as they are less disabling. Nevertheless, this malformation should be taken seriously due to its psychological impact on many women, from teenagers to those in their prime, who legitimately wish to address the issue to improve their self-esteem.
Understanding Tuberous Breasts
Tuberous breasts develop during puberty when breast growth occurs. They are believed to have a congenital origin but are not hereditary. The condition is characterised by abnormal mammary tissue that interferes with breast growth, likely due to irregularities in the mammary gland’s attachment to the pectoral muscle and skin.
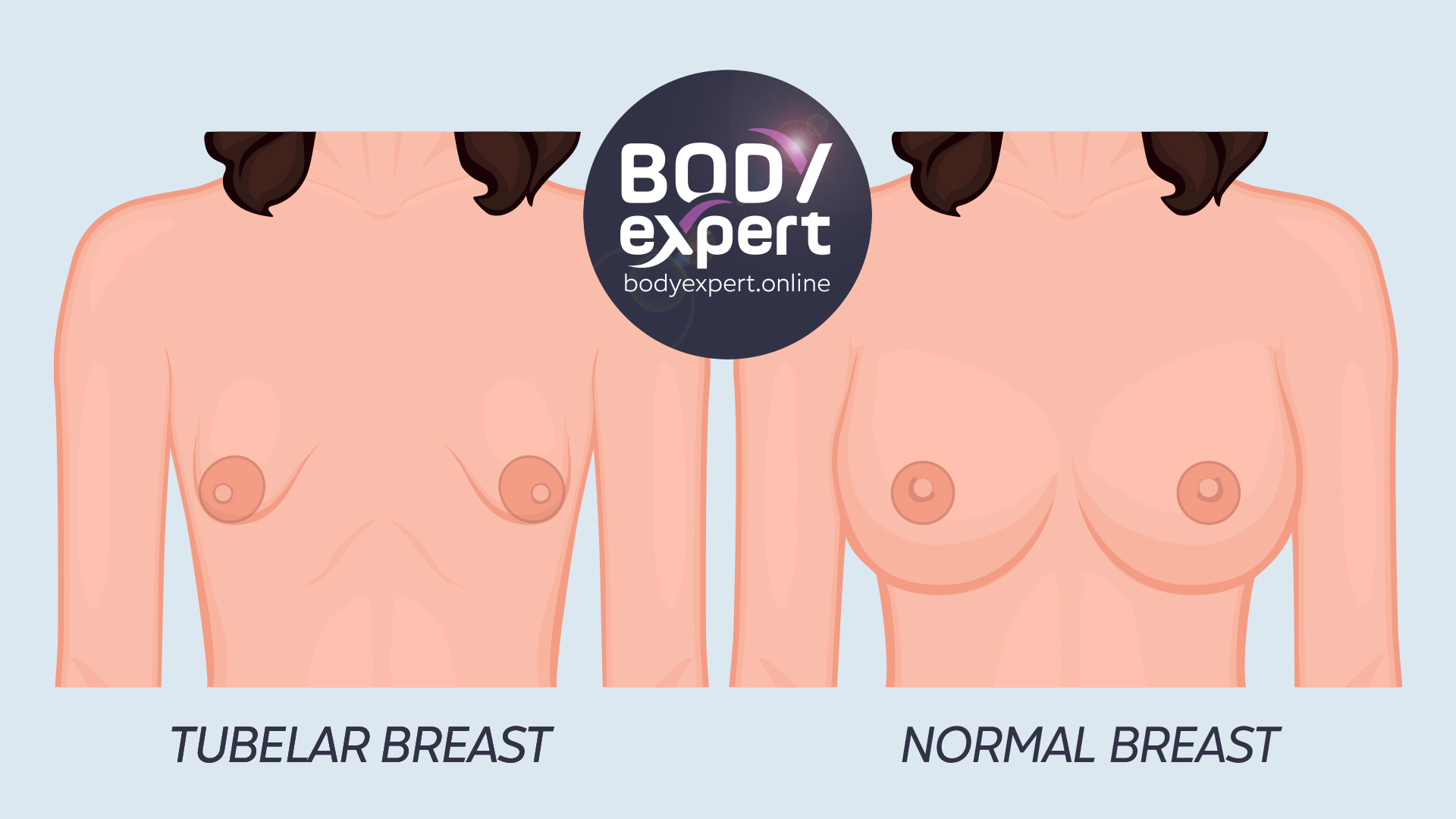
Key features of tuberous breasts include:
- A narrow pectoral implant base
- A large distance between the breasts
- Tube-shaped growth of the skin sheath
- A constrictor ring at the breast base impeding normal growth
- Often asymmetrical breasts (70% of cases)
- The appearance of insufficient skin with a marked neckline and stretch marks
- Generally large and protruding areolas due to glandular tissue herniation
Medical diagnostic protocols classify tuberous breasts into three stages of severity:
The 3 Stages of Tuberous Breast Severity
- Grade I: Considered benign, this level represents about half of all tuberous breast cases. The lower-internal quadrant of the breast is absent, with the areola pointing downwards and inwards. Surgical correction is relatively straightforward.
- Grade II: Characterised by a tube or funnel appearance, the two lower quadrants are absent, with the areola pointing downwards. Breast asymmetry is common. This stage accounts for approximately 25% of diagnoses.
- Grade III: The most severe stage, with all four breast quadrants absent. The protruding areola lacks support and epidermal volume, giving the breast a tube-like appearance falling downwards. Surgery for this type of malformation is the most complex.

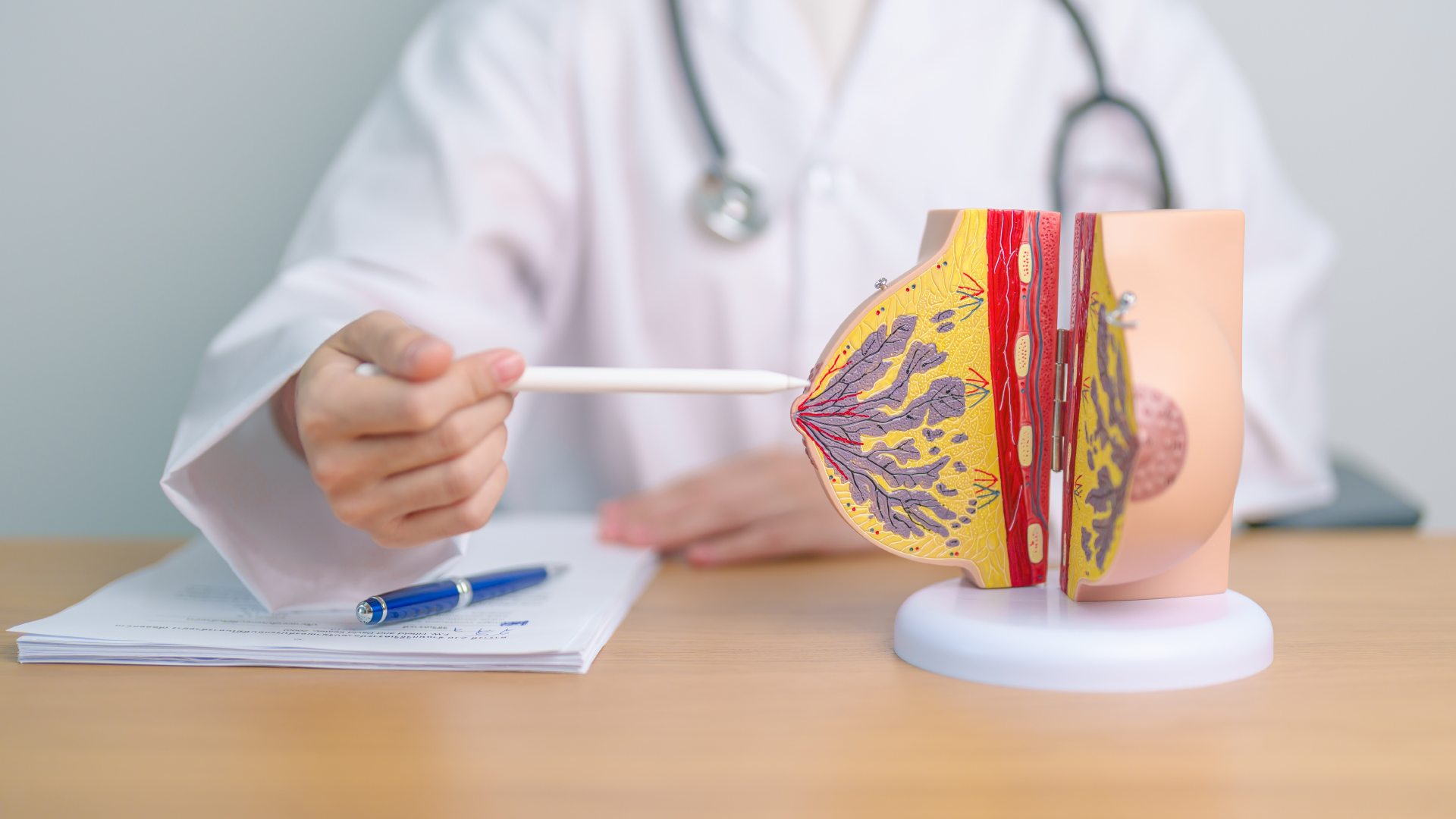
Diagnosis and Recommended Tests
Tuberous breasts can be diagnosed as early as adolescence. Any unusual changes in shape or abnormal growth should be reported. Self-examination can help identify initial signs, which should be confirmed by a GP, gynaecologist, or breast surgeon. It is advisable to wait until the end of puberty – or at least three years after the onset of menstruation – before considering reconstructive and cosmetic surgery.
Surgical Techniques for Correcting Tuberous Breasts
The goal of tuberous breast correction surgery is to address the diagnosed anomalies and create a more rounded, balanced shape for both breasts. Recent advances in breast lipofilling have made cosmetic breast surgery faster, more effective, and more reliable in the long term.
The surgical techniques employed depend on the grade of tuberous anomaly and may include:
- Simple mastopexy (breast lift) for Grade 1 tuberous breasts
- A combination of surgical techniques for Grade 3 anomalies

The surgical process typically involves:
- Two consultations with a specialist surgeon to determine the best approach
- A full medical examination, potentially including a mammogram or breast ultrasound
- An interview with the anaesthetist
- Adherence to pre-operative recommendations, such as stopping smoking and certain medications
The Surgical Procedure
Surgery for tuberous breasts is performed under general anaesthesia, requiring a minimum 24-hour hospital stay. The operation duration ranges from 40 minutes to 2 hours, depending on the complexity of the required surgery.

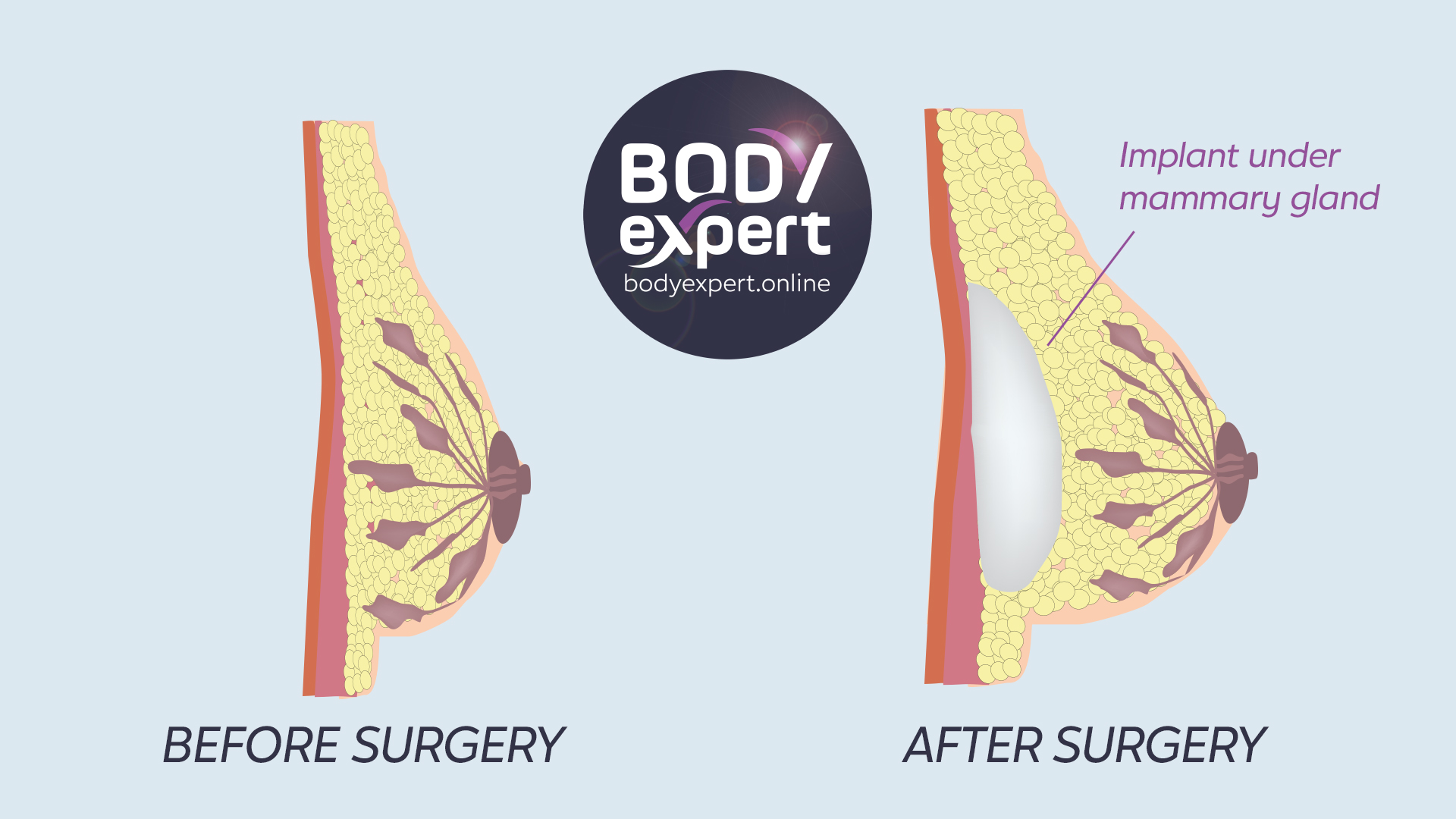
The main stages of the surgical approach include:
- Enlarging the breast base using an appropriately sized implant or expander
- Correcting the lower breast volume with lipofilling
- Repositioning the nipple and reducing the areola diameter if necessary
These steps are generally performed using a single incision around the areola.
Specific approaches for each grade:
Grade I: Treatment combines fasciotomies (breaking the fibrous ring with micro-needles) and breast lipofilling to reshape the breast and add volume. Areola reduction is often included.
Grade II: A breast lift (mastopexy) corrects the tuberous shape by removing excess skin and restoring curvature with lipofilling or breast implants. Areolar plasty may be performed to correct nipple size and asymmetry.

Grade III: This severe form requires two operations, 3-6 months apart. Treatment may involve sulcus-lowering plasty, ptosis cures, and breast plasty. Lipofilling and/or breast implants are essential for restoring volume and shape.
Post-operative Recovery and Care
Proper post-operative care is crucial for successful breast reconstruction. Key aspects include:
- Wearing a compression bandage for 24 hours after surgery
- Removal of healing strips between the 12th and 15th day post-operation
- Pain management with prescribed medications
- Limiting physical activities for several weeks
- Wearing a suitable support bra day and night for at least a month
The final result is visible about a year after the operation and lasts a lifetime, though natural changes due to weight fluctuations and ageing may occur.

Risks and Complications
While rare, potential risks and complications include:
- Haematoma, early irritation, scar infection, and bleeding
- Breast asymmetry, implant problems, scar hypertrophy, or nipple insensitivity
- Recurrence of the tubular breast shape, secondary areola enlargement, or the appearance of a double-fold

Comment évolue la sensibilité de la poitrine après chirurgie ?
Un engourdissement temporaire de la poitrine et des mamelons peut être généralement observé au cours des semaines suivant l’intervention, avant de retrouver leur sensibilité normale. La zone érogène des seins est totalement préservée.
Impact on Breast Sensitivity and Breastfeeding
Temporary numbness of the breast and nipples may occur in the weeks following surgery, but normal sensitivity typically returns. The erogenous zone of the breasts is preserved.
Tuberous breasts do not inherently disrupt breastfeeding, and corrective surgery may even improve the process by making areolas more accessible and skin more supple.

Cost and NHS Coverage in the UK
In the UK, tuberous breast correction surgery may be available on the NHS if it is deemed medically necessary. The NHS considers both physical and psychological factors when determining eligibility for breast surgery. For Grade II or III tuberous breasts, the psychological impact often justifies coverage.
To be considered for NHS funding, patients typically need to:
- Be referred by their GP to a plastic surgeon
- Meet specific criteria set by their local Clinical Commissioning Group (CCG)
- Demonstrate significant physical or psychological distress caused by the condition

If NHS funding is not available, patients may opt for private treatment. The cost of private tuberous breast correction surgery in the UK can range from £4,000 to £7,000, depending on the complexity of the procedure and the surgeon’s expertise.
Preparing for Tuberous Breast Correction Surgery
To ensure the best possible outcome:

- Consult with your GP about your concerns and potential NHS coverage
- If referred, choose a surgeon specialising in tuberous breast correction
- Review before-and-after photos of previous patients
- Read recommendations and opinions from past patients
- Obtain detailed information about the procedure and recovery process
- Discuss potential risks and complications with your surgeon
- If considering private treatment, obtain quotes from several specialists

2301 vues
0 commentaires
0






Il n'y a pas de commentaires pour le moment.