If not treated promptly, severe periodontal disease can lead to major oral health problems that are particularly challenging to resolve. Recognising the symptoms and causes of periodontitis is crucial for prevention, to avoid complications affecting the jawbone and the patient’s overall wellbeing. Early intervention also allows the most effective treatment plan to be put in place to save affected teeth.
Periodontitis, a chronic or aggressive inflammation of the gums leading to progressive destruction of the periodontium and loss of the tooth’s supporting structures, is one of the most prevalent dental diseases. The British Society of Periodontology estimates that around 50% of UK adults are affected by some form of gum disease. Without early treatment, periodontitis can progressively destroy a tooth and its surrounding bone until reaching an advanced stage, eventually causing tooth loss and complicating rehabilitation. Severe periodontal disease can lead to bone atrophy, preventing successful implant placement. Several therapeutic solutions exist to overcome this bone deficit, from All-On-4 or All-On-6 implant-supported prostheses to sinus lifts, bone grafts and zygomatic implants. While effective, these treatments are costly and not well covered by the NHS, leading many patients to consider dental tourism for affordable permanent solutions.

What is periodontitis and how does it progress?
Periodontal disease is a gum infection caused by bacteria. This microbial infection triggers inflammation in the tissues supporting the teeth, collectively called the periodontium. The periodontium consists of four components: 1) The alveolar bone, which surrounds the teeth and is part of the upper and lower jaws 2) The periodontal ligament, acting as a shock-absorber between the alveolar bone and tooth root 3) The gingiva (gums), which covers and protects the alveolar bone 4) The cementum, a layer enveloping the tooth roots that anchors them to the periodontal ligament
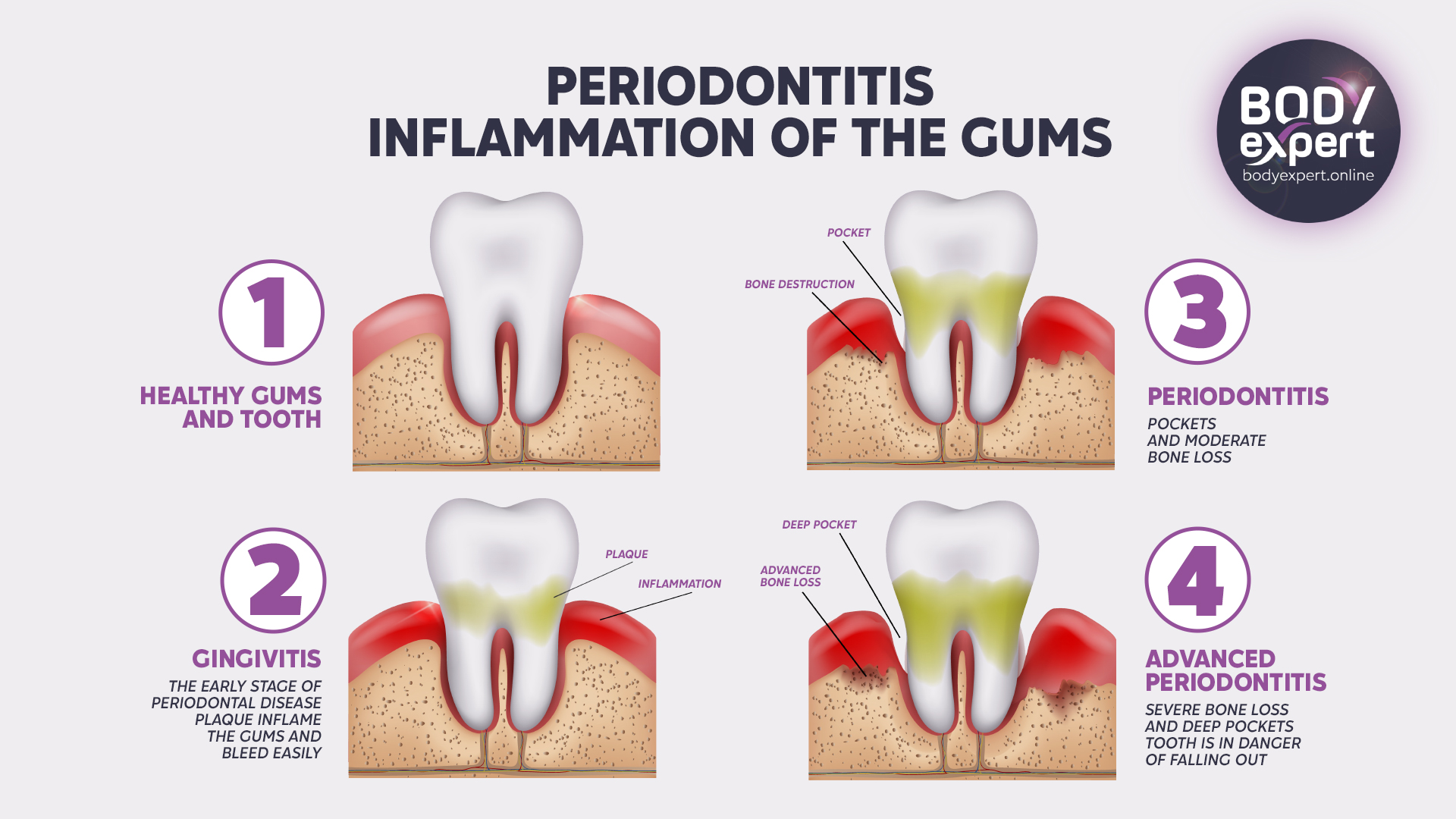
The bacterial assault initially causes inflammation of the gums, known as gingivitis. If not identified and treated quickly, gingivitis can advance to pulpitis, when infection reaches the tooth’s root, or periodontitis, when it spreads to the ligament and alveolar bone. Periodontal disease is common in adolescents and adults, with prevalence increasing with age.
Causes of periodontitis
This infection is primarily due to inadequate oral hygiene, allowing bacteria to accumulate between the teeth and gums. Over time, this leads to the formation of plaque – a sticky film on the teeth composed of salivary proteins, food particles (sugars and acids), and bacteria. As it calcifies, this white, opaque coating turns into tartar, potentially causing chronic infection. Along with visible plaque, early warning signs of periodontal disease include periodontal pockets, gum inflammation, and bleeding gums. Besides poor brushing habits, several other factors can exacerbate the onset of periodontal disease:

- A family history of periodontitis can help identify at-risk patients for prevention.
- Certain immunosuppressive diseases accelerate the development and persistence of periodontal infections by weakening the mouth’s defences.
- Age is a risk factor, especially from 55 onwards. Gum recession exposes the base of the teeth to tartar and bacteria accumulation.
- Dental malocclusion, whether inherited or due to injury, can contribute to chronic periodontal infections. Orthodontic treatment may be necessary.
- Smoking impairs the mouth’s immune response, reducing the gums’ natural protection and promoting the growth of harmful bacteria.
- A diet high in sugar and fat along with frequent consumption of sugary, acidic drinks increases oral acidity, encouraging bacterial proliferation in the oral tissues.
- Diabetes favours the development of periodontal disease and vice versa. Elevated blood sugar levels promote the formation of dental plaque and its associated bacteria, which feed on glucose in saliva. Dry mouth combined with excess carbohydrates and plaque encourage tooth decay, particularly in diabetic children. Diabetes also destroys collagen, a protein essential for healthy gums, tendons and bones. It contributes to blood vessel inflammation, reducing blood flow to the gums and weakening them.

Progression of periodontitis
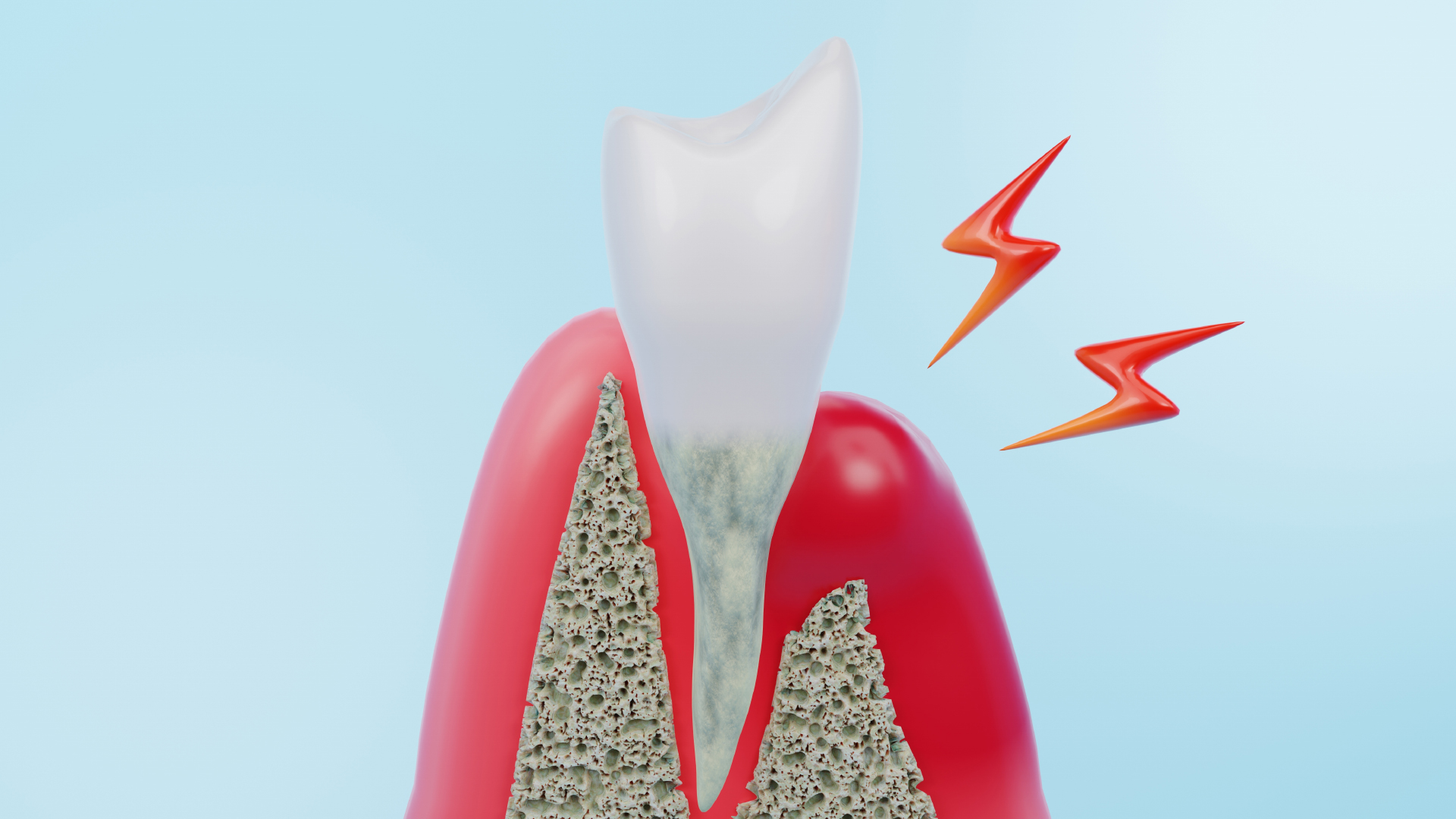
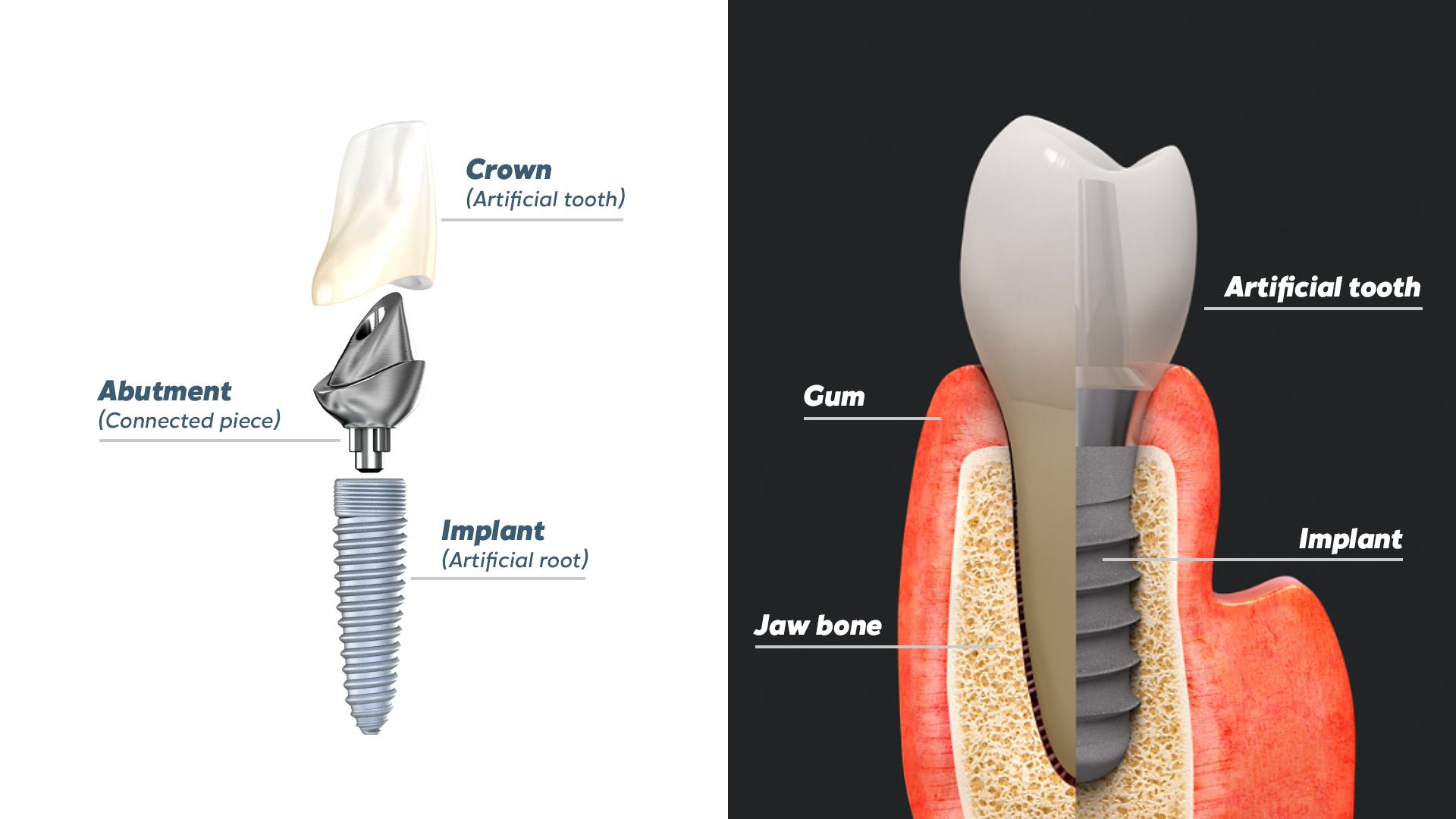
Following gingivitis, bacterial infection of the gum tissue affects the tooth-supporting structures, leading to worsening periodontal disease. As the gums and alveolar bone recede, periodontitis becomes chronic and the tooth loses stability. Without proper treatment, the bone continues to deteriorate. In advanced periodontitis, the tooth is no longer anchored by the periodontium and eventually falls out. At this end stage, periodontitis can no longer be reversed. Extraction of the infected tooth becomes necessary, with replacement by an implant-supported prosthesis. In the absence of an active tooth, the bone is no longer stimulated and continues to shrink, while infection persists in the periodontium of adjacent teeth.
Research highlights the difficulty of classifying periodontitis as a single disease with variations or as distinct conditions. However, evidence suggests there is no clear basis for differentiating chronic and aggressive periodontitis. Periodontologists do distinguish different stages of progression though: periodontitis, necrotising periodontitis, and periodontitis as a direct manifestation of systemic diseases (immunosuppressive illnesses, depression, HIV, diabetes, etc.).
Recognising symptoms at different stages
Never ignore a toothache, as it could indicate periodontitis, which consistently leads to chronic disease progression if untreated. In the early stages, the main warning signs of periodontitis are:
- Bleeding gums
- Sensitivity to hot and cold
- Tender, hypersensitive gums
- Soft, spongy gums
- Gum recession and/or swelling
- Bad breath
If a patient notices any of these symptoms, they should see a dentist immediately for diagnosis and to determine the level of disease progression. In advanced or necrotising stages, additional symptoms can be readily detected:
- Intense pain in the tooth roots
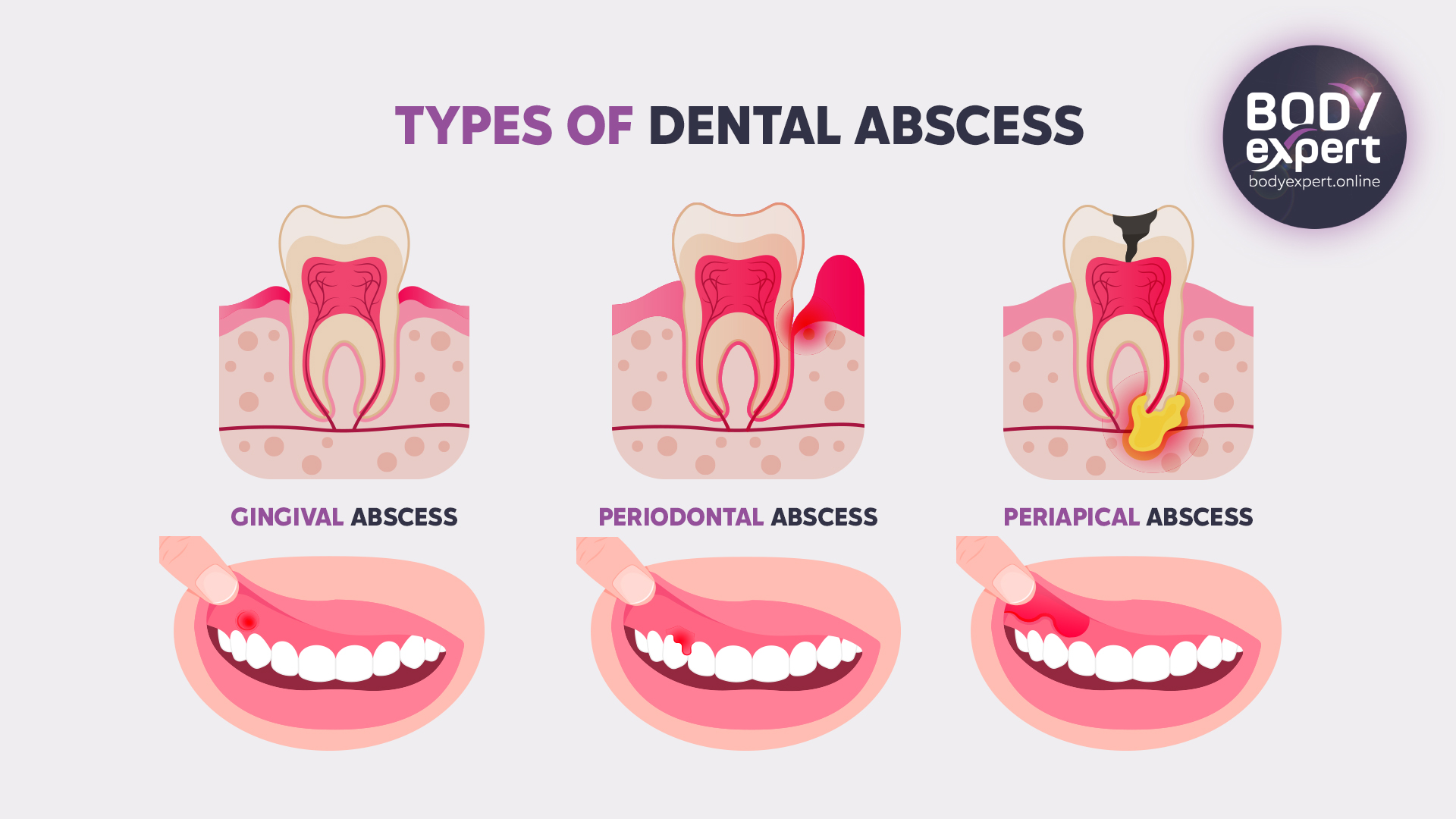
- Periodontal abscesses and pus at the gum line
- Loose teeth
- Persistent bad breath
- Tooth loss

Consequences of severe periodontal disease
Left untreated, end-stage periodontitis means the infected tooth can no longer be saved. Permanent tooth loss has serious repercussions for the patient’s oral health. Beyond causing recurrent pain and infection, periodontitis can spread to neighbouring teeth, accelerating the patient’s progression to edentulism. This directly impacts food mastication and thus overall eating habits, as well as speech. It also leads to aesthetic concerns, with psychological consequences for the patient’s confidence and self-esteem.
Moreover, severe periodontal disease can have grave implications for the patient’s general health, including heightened cardiovascular disease risk and worsening of diabetes in affected individuals.

Treatment approaches for advanced periodontitis
Non-surgical methods
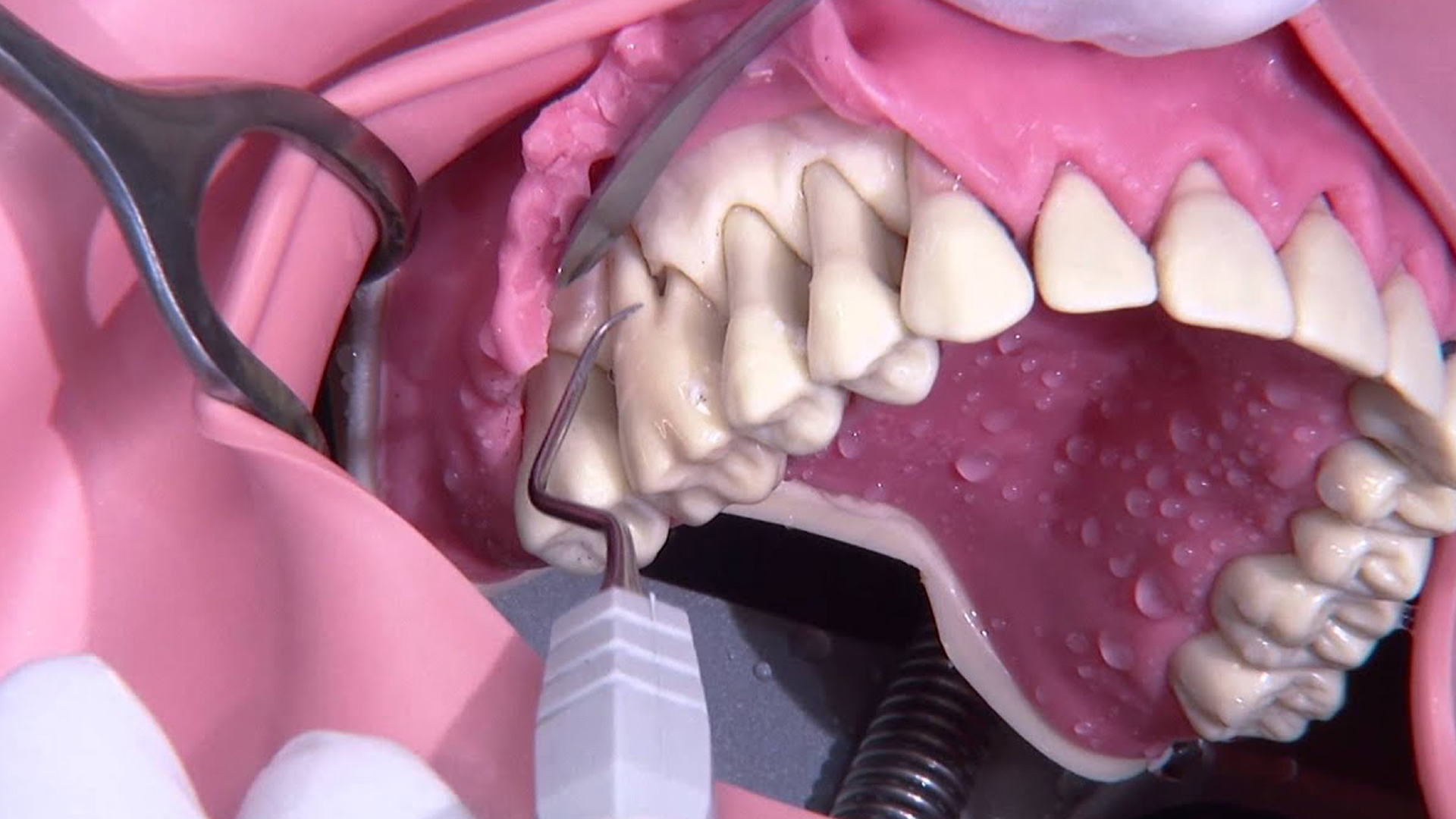
Supra- and subgingival scaling
Subgingival scaling, or root planing, removes tartar deposits on and beneath the gum tissue without damaging the tooth enamel and pulp. Any detected decay or pulpitis must be treated to prevent the infection progressing to apical, chronic or acute periodontitis. Performed under local anaesthetic, this minimally invasive procedure involves several steps: curettage (manual or ultrasonic), root surfacing and smoothing, followed by a final rinse. Subgingival scaling allows the periodontal pocket – the space opened up between gum and tooth by periodontitis, where bacteria colonise – to be eliminated. If deep cleaning and surfacing prove insufficient, periodontal surgery becomes necessary.
Antibiotics may be prescribed alongside non-surgical treatment to prevent the infection from spreading. Crucially, patients must follow their dental surgeon’s oral hygiene instructions to the letter, brushing three times daily for at least 2 minutes each time. Using a soft-bristled toothbrush to avoid gum inflammation, along with interdental brushes, floss or a water flosser, ensures thorough cleaning between each tooth to prevent plaque formation and bacterial persistence in these crevices.

Periodontal surgery
When periodontitis is too advanced, periodontal surgery may be indicated. Several techniques can be employed to treat and halt the disease before it reaches the terminal stage.
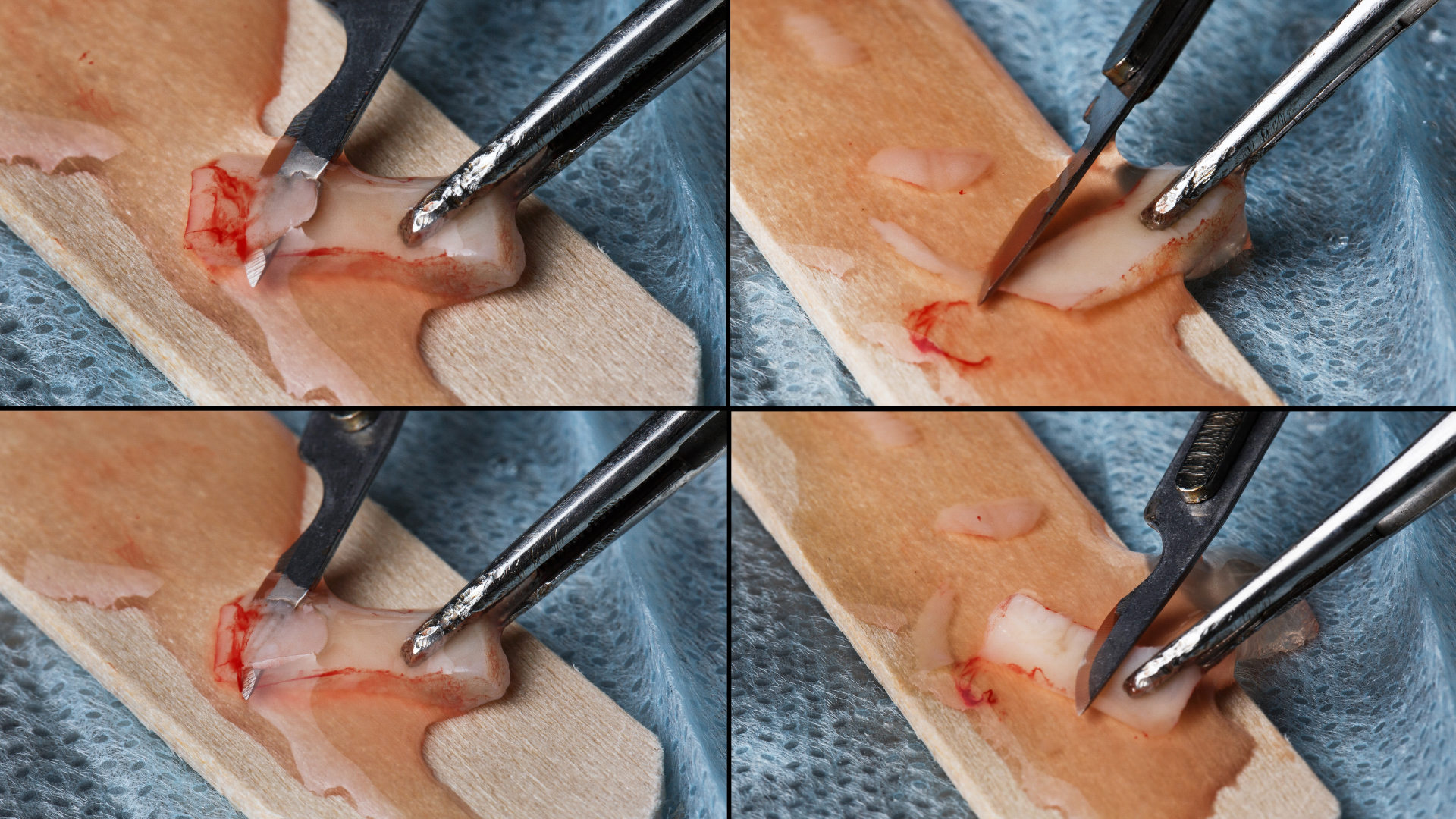
Flap surgery
Effective for eliminating tartar and bacterial deposits at the tooth base, flap surgery involves opening up the gum tissue in flaps to access the tooth roots and alveolar bone. Carried out under local anaesthetic, it requires stitches to reposition the gum and promote healing. This treatment thoroughly cleans the periodontium and removes tartar and bacteria. However, the post-operative fragility of the treated area means patients must be cautious when chewing and eating, and when cleaning their teeth, which may be mobile due to lack of gum support. After surgery, the gums recede and swell as they heal.
Periodontal pocket reduction
Periodontal pocket reduction or filling surgery, also called gingivectomy, refers to a group of surgical procedures used to clean plaque and bacteria from the root of an infected tooth by reducing periodontal pockets. It slows pocket infection and inflammation while curbing alveolar bone destruction caused by periodontitis. It also facilitates daily tooth cleaning, allowing patients to brush the base of their teeth more effectively, thus reducing the risk of new periodontal infections. Usually performed under general anaesthetic, the gums are flattened and sutured with micro-stitches post-operatively, before applying an antibacterial gel and potentially prescribing antibiotics.

Gum grafts
When a dental surgeon observes significant gum recession in a patient with severe periodontitis, they may recommend a gum graft to restore lost gingival height or thickness. Gum tissue, typically harvested from the roof of the patient’s mouth, is grafted onto the receded area around the infected tooth. This simple, quick, minimally invasive procedure, done under local anaesthetic, covers the exposed root and thickens the gum while reinforcing tooth support, ensuring its long-term protection and stability. Gingival grafting also helps the patient regain a harmonious smile with more even gum alignment.
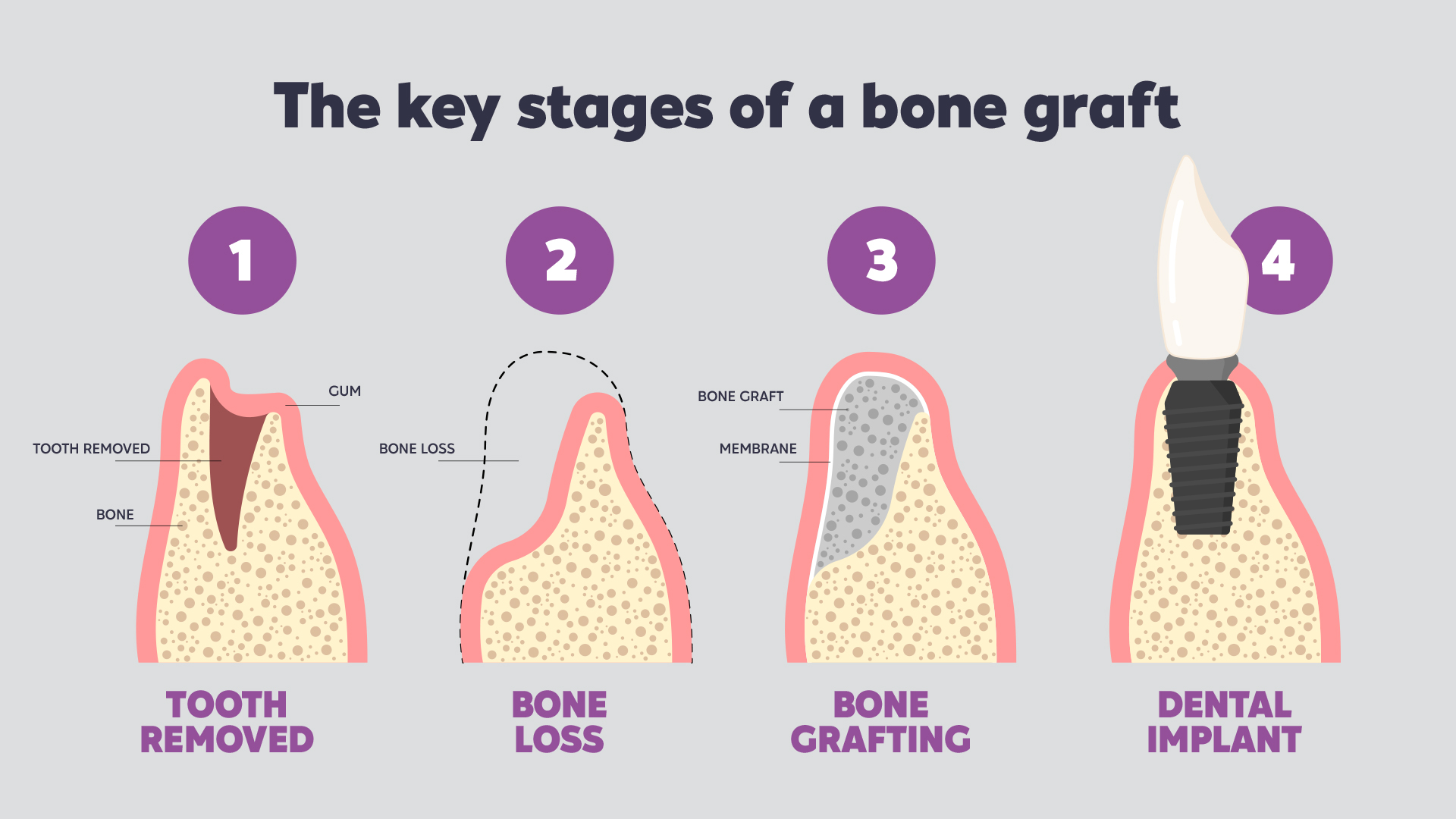
Bone grafting or filling
One consequence of periodontal disease is reduced bone mass around the teeth. The bone shrinks due to the combined action of bacteria and lack of chewing activity caused by pain from the dental infection. When this bone volume is insufficient for placing an implant-supported dental prosthesis, bone grafting compensates for the deficit and ensures the long-term success of implant therapy. X-rays assess the bone tissue characteristics and calculate the required graft volume. Performed under local anaesthetic, the graft usually uses biocompatible synthetic bone. A healing period of several weeks is typically necessary before implant placement to ensure graft integration.
Recent innovations
Thanks to new technologies in the medical field, several recent innovations have enabled the development of less invasive techniques for treating periodontitis.
Laser treatment
Laser treatment allows highly effective, minimally invasive disinfection of periodontal pockets and elimination of bacteria compared to surgery, while stimulating gum cells. This biostimulation technique increases blood circulation and accelerates the formation of collagen fibres and bone cells for much faster healing and tissue repair. Performed after scaling and root planing, laser cleaning generally requires multiple low-intensity sessions.
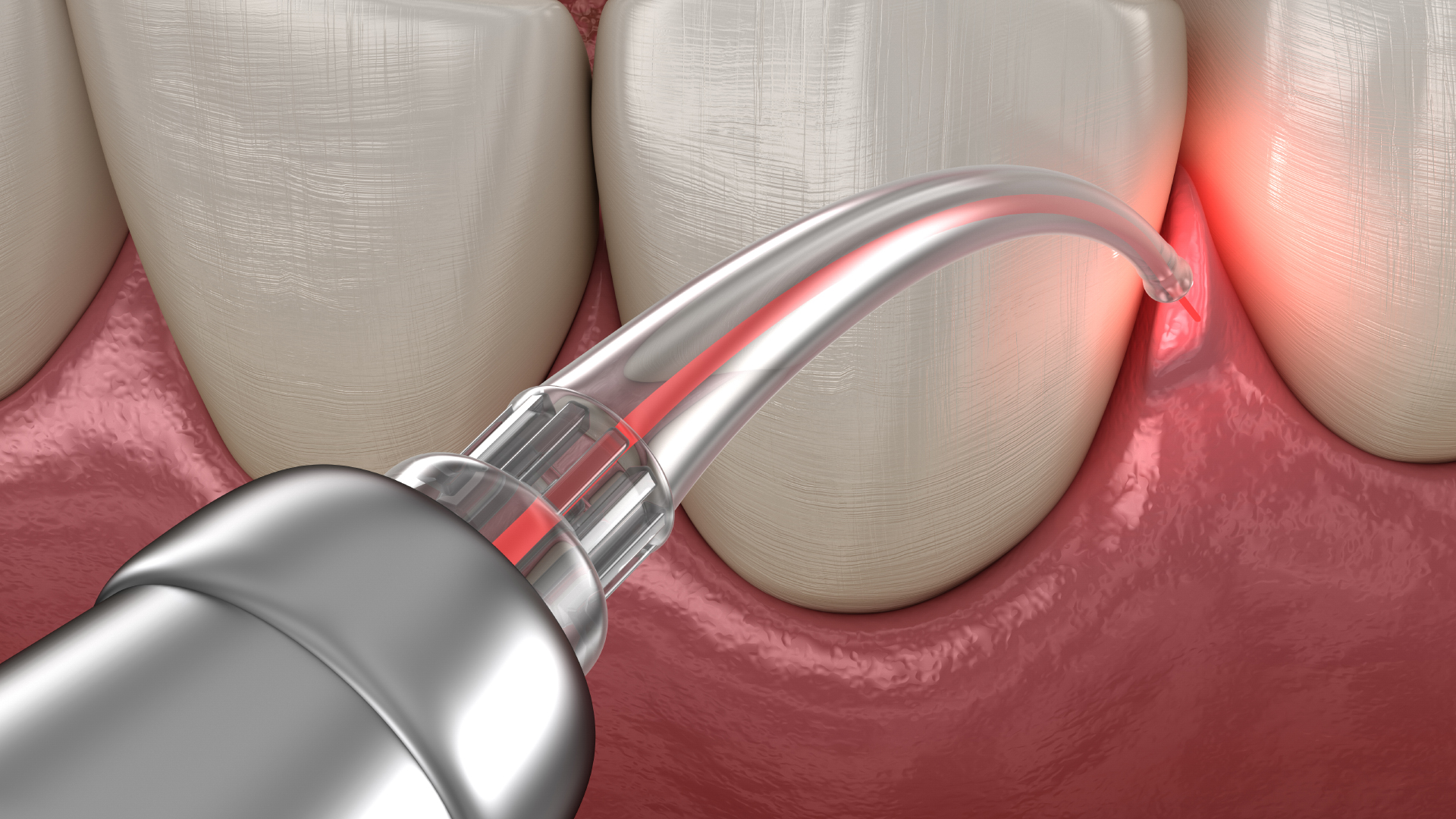
Photodynamic therapy
This promising new technique, recently introduced in dentistry, is also known as light therapy. As a local anti-infective treatment, photodynamic therapy has proven effective against dental plaque bacteria, especially antibiotic-resistant strains. Its rapid action, low cost, ease of use, and lack of side effects make it a highly promising approach. Under light radiation of a specific wavelength, a photosensitising agent is activated, interacting with surrounding biological molecules via electron transfer and with oxygen via energy transfer. These reactions generate highly reactive free radicals that destroy the targeted bacteria. Red light from a diode laser is transmitted through a thin, curved optical fibre easily inserted into periodontal pockets, diffusing light deep into the tissues.

Guided tissue regeneration
This technique regenerates the bone volume lost during periodontal disease. Preceded by cleaning with a diode laser, which decontaminates 99% of bacteria in the treated area while stimulating blood and bone cell growth, this method combines bone filling with the introduction of hormonal growth factors to stimulate bone regeneration in the infected site.

Saving or extracting a tooth with severe periodontitis?
When a tooth is damaged by periodontal disease and its integrity is threatened, the dental surgeon must choose between preserving the infected tooth and extracting it in consultation with the patient. For the dentist, extracting the tooth and replacing it with an implant-supported prosthesis is the simplest, quickest, most cost-effective solution. However, in both medicine and dentistry, organ preservation and conservative treatment should remain the priority, especially given the proven long-term efficacy of currently available periodontal techniques.

Faced with severe cases where the patient’s poor oral hygiene is evident and their suffering becomes unbearable, dental surgeons must nevertheless be wary of “preventive extraction”, a frequently favoured approach. They should retain the best possible analytical skills to establish a specific prognosis for each tooth while considering the potential for comprehensive therapy. Preventive extraction is indeed tempting: tooth survival after periodontal treatment is less predictable and lower than that of an implant-supported prosthesis. Artificial teeth have lower complication rates than periodontally involved natural teeth, and their cost-benefit ratio and aesthetic outcomes are superior to periodontal treatment. Consequently, patients are often more satisfied with their new prosthetic teeth, although they must still maintain rigorous hygiene to ensure their long-term quality.
While medical research generally favours preserving teeth whenever possible, even with severe periodontitis, the patient bears significant responsibility for the survival of a periodontally treated tooth. Without meticulous oral hygiene, the longevity of a treated tooth is no better than that of an untreated tooth. Aggravating factors may also be present: smoking, family history, or uncontrolled diabetes, for example, all favour an artificial solution, which is always easier to implement than overcoming an addiction or a genetic or hormonal imbalance. The practitioner then faces a crucial question in establishing their prognosis: will my patient be able to withstand the treatment and stabilise their periodontal disease?
Periodontitis and orthodontic treatment
Orthodontic treatment has a beneficial long-term effect on patients’ periodontal health. The combination of orthodontics and periodontics helps realign teeth, reduce crowding, correct malocclusions, and harmonise the dental arches, making tooth brushing more effective – the foundation of good periodontal health. Malocclusions can actually worsen the onset of periodontitis, as bacteria settle between the bases of misaligned teeth. Orthodontic treatment, prescribed from pre-adolescence onwards, can prevent periodontal disease from appearing in adulthood. Conversely, the absence of orthodontic intervention can encourage the onset or worsening of periodontal disease. Periodontal surgery combined with rigorous hygiene reduces inflammation of the periodontium and promotes cementum, ligament, and bone formation when combined with orthodontic forces. Orthodontic treatment helps halt the disease, regenerating the periodontal tissues over the long term.

Preventing and raising awareness of periodontitis
Excellent oral hygiene
To prevent periodontal disease, rigorous dental hygiene is essential, combined with the regular use of tools to help prevent bacteria from permanently settling in the periodontium: brushing three times a day for two minutes each time, using a soft toothbrush and a toothpaste with natural, non-aggressive ingredients, and using various instruments for the interdental areas where bacteria tend to accumulate (dental floss, water flosser, interdental brush, etc.). But there are other factors that can positively influence patients’ dental health and help prevent periodontitis.

Quit smoking, limit sugar
Smoking, an unbalanced diet rich in sugars and fats, sugary and/or acidic fizzy drinks, and alcohol consumption are aggravating factors, as they weaken the gums and erode the periodontal zone, while coffee and tea encourage the formation of dental plaque.
Regular check-ups and early detection
It is essential for every patient, even those with impeccable oral hygiene, to visit the dentist at least once a year. Plaque, a mixture of tartar and bacteria, can build up despite regular brushing, and annual scaling is crucial.

Parents have a special responsibility and a fundamental role to play in preventing periodontal disease in their children. A child who practises good oral hygiene and consumes few sugary and fizzy drinks will be able to maintain healthy teeth in the long term and prevent the onset of periodontitis. For children too, regular dental visits allow early detection of gingivitis or pulpitis.
Why treat severe periodontal disease in Turkey with Body Expert?
In cases of severe periodontitis, diagnosed by your regular dental practice, ortho-periodontal treatment abroad may be considered. Periodontal surgery, bone grafts, and the placement of implant-supported prostheses are poorly covered by the NHS, and dental clinics in the UK often charge high fees. Not to mention the delays, sometimes several weeks or months, in obtaining a treatment appointment – an untenable situation when severe periodontitis is causing paralysing pain, threatening your general health, disrupting your daily life, and undermining your psychological wellbeing.

In Turkey and Hungary, two leading destinations for European dental tourism, dental and periodontal clinics offer prices 60-80% lower than in the UK, with equivalent or even superior quality of care. Appointments can be made very quickly, and treatment carried out within 2-5 days. As long as you carefully choose your providers, they will offer all the legal guarantees of care and post-operative follow-up.

Choosing Body Expert in Turkey for treating severe periodontal disease
- Excellence in periodontal care: At Body Expert, dental clinics and specialist surgeons offer expertise in managing all forms of periodontal disease in a comfortable, secure setting with personalised care.
- Advanced technologies: The clinics selected by Body Expert are equipped with the best diagnostic and treatment technologies available in dental surgery: digital imaging, lasers for periodontal therapy, and all innovations that improve treatment efficiency and patient comfort while reducing healing times.

- Affordable costs: Turkey offers the best value for money for British patients, with prices two to three times lower than domestically, and a quality of care that is equivalent if not superior, allowing high-quality dental treatment to be democratised.
- Comprehensive care and support in English: Body Expert provides personalised assistance for its patients, from the initial application through to post-operative follow-up. All care is provided in English, offering a comfortable and reassuring treatment pathway.
- No waiting: Body Expert doesn’t keep patients waiting and can organise care within very short timeframes.
Opting for dental treatment in Turkey with Body Expert also means choosing a VIP experience in a magnificent setting. Body Expert takes care of the complete organisation of your stay, allowing you to concentrate on healing while enjoying Turkey’s touristic, gastronomic, cultural and natural riches.
4962 vues
0 commentaires
0






Il n'y a pas de commentaires pour le moment.