Periodontitis stands among the top conditions compromising human dental health. As common as cavities, yet not as widely acknowledged, periodontitis silently advances beneath the gums. When inflammation causes gums to recede around teeth, when tartar mars their base, and when chewing triggers discomfort, periodontitis is likely the stealthy culprit. The French Dental Association reports that half of the French population battles periodontal diseases.

What is Periodontitis?
Periodontitis pertains to afflictions that target the periodontium. This vital structure, composed of gums, root cementum, periodontal ligament, and the alveolar bone that cradles dental roots, can succumb to various inflammatory and bacterial onslaughts.
The fallout of periodontal diseases is multifaceted, inflicting harm not only on dental health but also on overall well-being:
Dental plaque formation, a precursor of chronic infections;
- Tooth mobility from gum recession, possibly culminating in alveolar bone resorption and tooth loss;
- Functional pain during mastication, impairing digestion quality;
- Heightened cardiovascular risks (heart attacks, strokes), due to systemic infections via inflammatory molecules and bacteria;
- Exacerbation of diabetes;
- Increased likelihood of liver and intestinal diseases, potentially leading to intestinal inflammation and colorectal cancer;
- For expectant mothers, the stakes are higher, encompassing pregnancy complications like miscarriage and premature birth, particularly due to hormonal fluctuations.

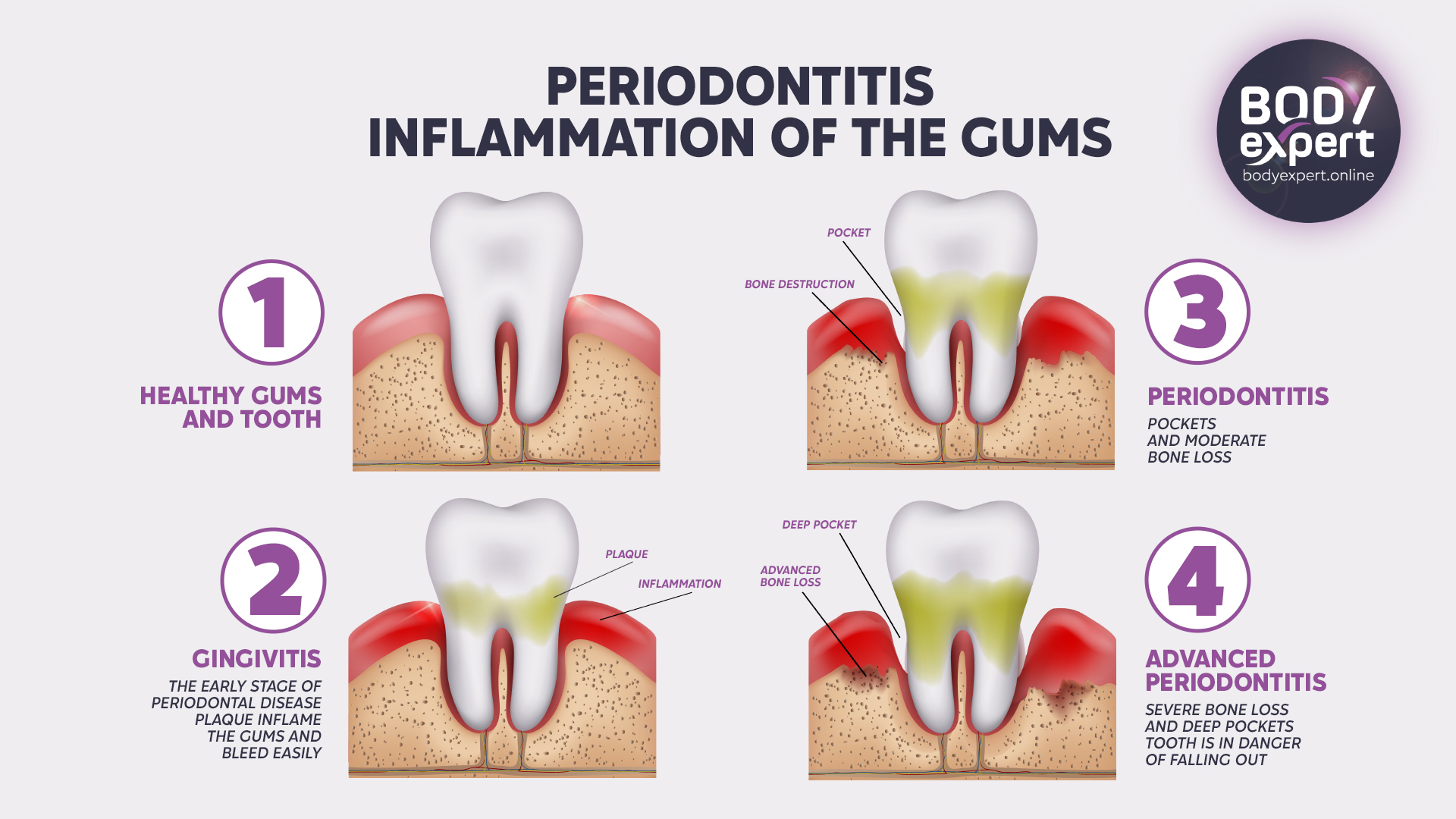
Gingivitis vs. Periodontitis: Understanding the Difference
Gingivitis is essentially periodontitis’ precursor. Addressing gingivitis promptly and effectively can ward off its progression to periodontitis.
Gingivitis manifests through a few tell-tale signs: gum redness, sensitivity, bleeding during brushing, swelling, and persistent bad breath. The solution isn’t complicated: professional teeth cleaning or scaling, biannually, coupled with diligent oral care.
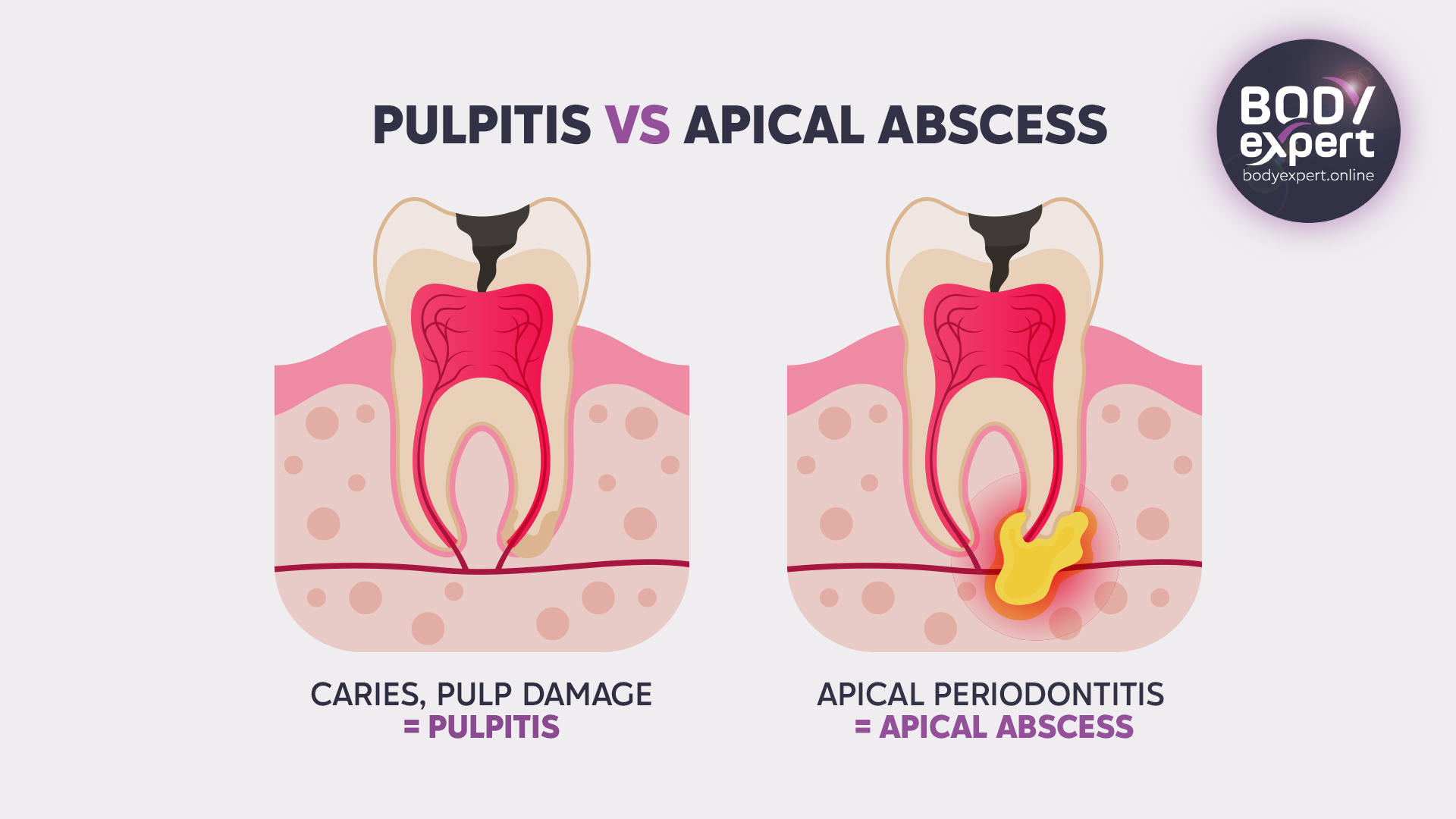
A dental consultation is imperative for the first signs of gingival discomfort (such as inflammation or redness). A dentist can intervene quickly with treatments like planning or scaling to heal gingivitis and avert periodontitis. Yet, it’s important to recognise that some forms of periodontitis, like apical periodontitis, might arise from improperly treated cavities, even without apparent gingival inflammation.

What’s the Difference Between Gingivitis and Periodontitis?
Gingivitis is frequently thought of as the precursor to periodontitis. With early and proper treatment, gingivitis can be managed, preventing its progression to periodontitis.
Gingivitis is characterised by a number of clinical symptoms: gum redness, sensitivity, bleeding during brushing, swollen tissue around the teeth, and halitosis (bad breath). The solution is straightforward: regular dental cleanings (ideally twice a year) and diligent oral hygiene can mitigate these symptoms.
When signs of gum pain emerge, such as inflammation or redness, prompt consultation with a dentist is crucial. They can intervene quickly with procedures like planning and scaling to treat the gingivitis and stop periodontitis from developing. In contrast, some forms of periodontitis, like apical periodontitis, can develop due to inadequately treated tooth decay, which might occur without any obvious signs of local gingival inflammation.
What Causes Periodontal Disease?
The leading cause of periodontal disease is typically poor dental and oral hygiene. However, certain aggravating factors have been identified by medical and dental research:
- A patient’s family history can often aid in recognising and even preventing the initiation of periodontal disease.
- Immunosuppressive conditions can promote the emergence and persistence of periodontal infections, primarily due to a compromised immune defence in the mouth.
- Age is another contributing factor, especially after 55, when receding gums expose the tooth’s base, leading to tartar and bacteria accumulation.
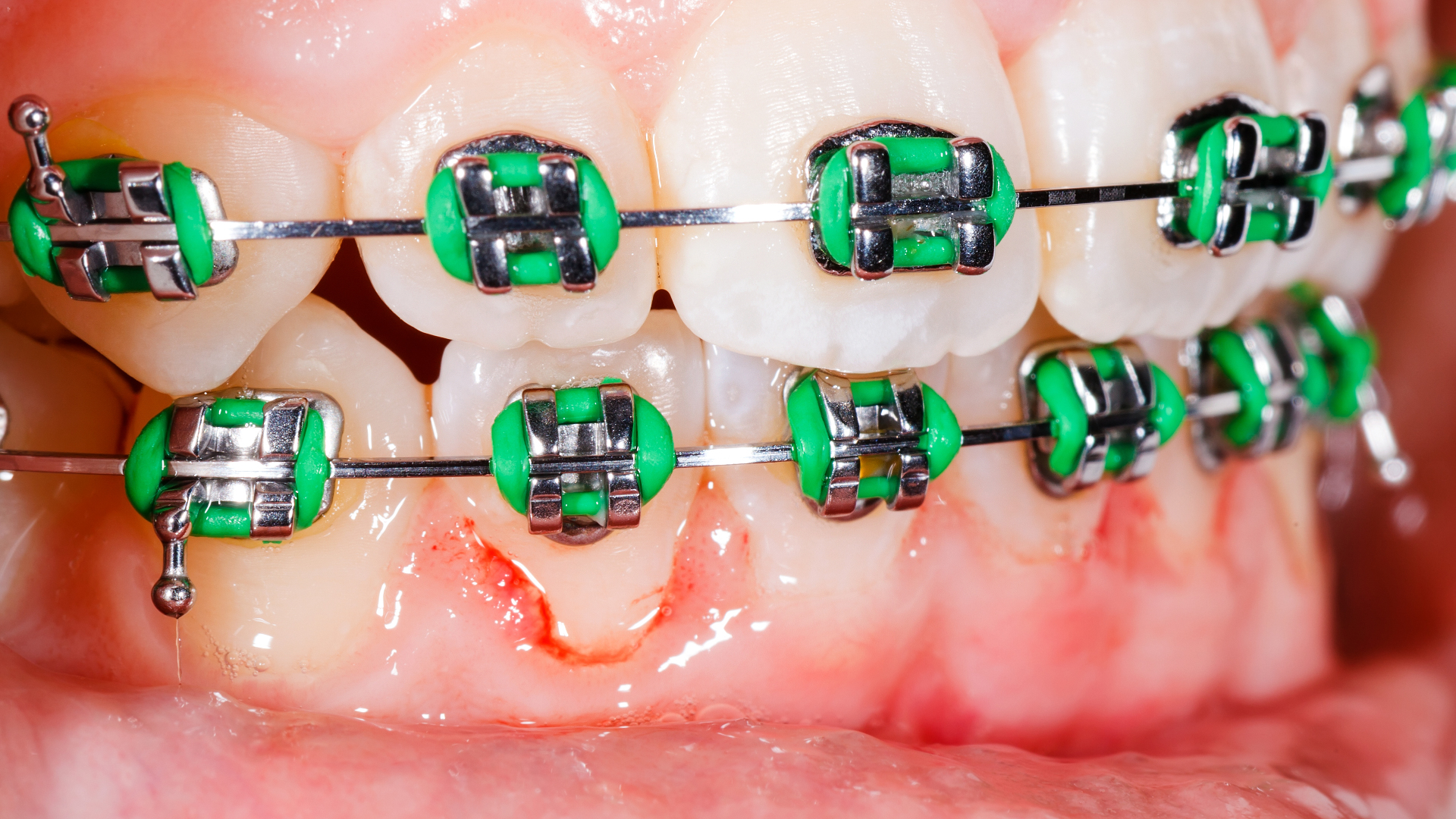
- Whether inherited or caused by an accident, poor tooth alignment and dental malocclusion can lead to chronic periodontal infections. Orthodontic intervention may be necessary to address these periodontal challenges.
- Tobacco use also fosters periodontal disease by attacking the mouth’s immune defences, diminishing the gums’ natural protection, and promoting harmful bacteria that deteriorate the periodontium.
- Diets high in refined sugars and carbohydrates—the enemies of periodontal health—can alter the mouth’s pH, encouraging oral bacteria growth. Overconsumption of sugary carbonated drinks and fatty foods dramatically increases mouth acidity and bacterial proliferation.

Diabetes and Periodontitis: A Harmful Combination
The relationship between diabetes and periodontal disease is a particularly harmful one, as they tend to exacerbate each other. Individuals with diabetes experience a noticeable decrease in salivary flow, paving the way for an increase in oral microbes since saliva is a natural defence against bacteria. The glycemic irregularities that come with diabetes promote the growth of dental plaque and its bacteria, which thrive on the glucose in saliva.
A dry mouth, along with an overabundance of carbohydrates and dental plaque, leads to an increased risk of tooth decay, especially in children with diabetes.
Furthermore, medical research has demonstrated that diabetes contributes to collagen breakdown in the gums. As a crucial protein for the integrity of gum tissue, tendons, and bones, weakened collagen creates a favourable environment for periodontal disease. Moreover, the diabetic-related inflammation of blood vessels reduces blood flow to the gums, further compromising their health.

The two conditions are intricately connected: Research has found that individuals with type 1 diabetes are 3.5 times more prone to developing periodontal disease compared to those without diabetes. Those with type 2 diabetes face a 2.8 times higher risk, and patients with periodontitis are twice as likely to develop type 2 diabetes. This link may be due to bacterial lipopolysaccharides (LPS), common in periodontal disease, that contribute to systemic inflammation and, as a result, increase the likelihood of developing type 2 diabetes.
Why Choose Body Expert and Turkey for Periodontitis Treatment?
- Top-Tier Periodontal Services: Turkey is renowned for its cutting-edge dental facilities and proficient periodontists. Body Expert boasts a team of specialists adept in correcting various periodontal issues, employing the most recent breakthroughs to ensure superior outcomes.
- Cutting-Edge Technology: Clinics in Body Expert’s network are outfitted with the latest in diagnostic and therapeutic tech. Innovations such as digital imaging and lasers for gum treatment enhance the efficacy of care, maximise patient comfort, and expedite recovery.
- Cost-Effective Solutions: The financial aspect of periodontitis care can be daunting, yet Turkey presents a cost-effective alternative. With prices notably more budget-friendly than in many other nations, progressive periodontal therapies become more accessible.
- Effortless French Language Support: Recognizing the need for clear communication and solid support, Body Expert extends comprehensive assistance in French. This covers every phase, from the preliminary assessment to aftercare, fostering a seamless and informed journey for French-speaking clients.
- No Delays: With Body Expert’s preferred Turkish clinics, patients can receive immediate attention for their periodontitis, sidestepping the usual wait times.
Beyond the treatment itself, selecting Turkey offers a unique chance to recuperate amidst splendid surroundings. Body Expert meticulously arranges your visit, ensuring patients can focus on healing while also experiencing Turkey’s rich cultural and natural splendour.
How Can Periodontitis Be Prevented?
Embracing the adage that prevention is better than cure is key in periodontitis. Establishing a robust dental and oral hygiene routine is essential. This includes brushing teeth three times a day, using gentle, plant-based toothpaste, and a soft toothbrush to avoid causing harm to the gums. Patience and thorough brushing, especially around the base of the teeth and the gum line, will go a long way in maintaining oral health and warding off gum and periodontal diseases. It’s also vital not to overlook the spaces between teeth, utilising tools such as interdental brushes, dental floss, or water jets to combat tartar formation and bacterial buildup.

Diet plays a significant role in oral health, with sugars, carbohydrates, and tobacco being detrimental. Even tea and coffee can contribute to tartar accumulation and staining. Thus, mindful eating and oral care after meals or drink breaks is important.
Reducing sugar intake, especially from sources like glucose syrup and acidic carbonated drinks, is advisable, as these can damage and weaken the gums and periodontal tissues. It’s not just about cutting out sugar but also about choosing healthier options and ensuring good oral hygiene after consumption.
Some orthodontic conditions, including malocclusions, may worsen the risk of developing periodontitis, as they create niches where bacteria can thrive at the base of misaligned teeth. Beginning in adolescence, orthodontic treatments can rectify these issues and help prevent periodontal disease later in life.

Periodontitis Treatment Explained
Periodontics, a dedicated branch of dentistry, addresses the health of the periodontium. Upon diagnosing periodontitis, treatment varies based on severity and is typically conducted by a periodontologist. This specialised field requires an additional 3 to 4 years of training beyond general dental studies. Both general dentists and periodontologists begin treatment with a thorough periodontal examination. Most cases of periodontitis respond well to initial treatments such as scaling and root planing, but advanced infections might necessitate surgery or dental prosthetic interventions.

The Process of Scaling and Subgingival Cleaning
Scaling is performed to eradicate plaque and tartar, followed by an in-depth cleaning of the gingival pockets and the areas beneath the inflamed gums. This process allows for comprehensive cleaning of the gum tissue, thereby minimising infection risks. Root planing or subgingival scaling meticulously removes tartar deposits both above and below the gum line, preserving tooth enamel and pulp integrity. Concurrently, any present decay should be addressed, particularly to avert chronic or acute apical periodontitis.
This procedure can entail multiple visits and is divided into various stages under local anaesthesia: curettage (by hand or ultrasonic), surfacing and smoothing of the teeth, and finally, rinsing. Subgingival scaling aims to shrink the periodontal pocket—the space created by periodontitis between the gum and tooth where bacteria flourish—preventing the tooth from becoming loose.
Should deep cleaning and resurfacing fall short, surgical intervention might be the next course of action.

The Various Periodontal Diseases and Their Treatment
Periodontitis is an overarching term, but it comprises several distinct conditions that require a specific medical approach. Some of these diseases are only detectable with advanced dental technology, such as 3D scans, periapical X-rays, or panoramic X-rays.
Apical Periodontitis: The Most Insidious Form of Periodontitis
Apical periodontitis is an inflammatory lesion deep within the peri-radicular periodontium caused by a bacterial infection within the tooth’s interior (endodontium). This often stems from decay that hasn’t been adequately addressed, allowing the infection to travel down the root canal to the root tip over the years. An infectious abscess can form where the root connects with the periodontal bone—the apex—causing nerve inflammation.
Chronic apical periodontitis tends to manifest with sharp, intermittent pain as the inflammation slowly progresses, making it more challenging to detect. It’s characterised by gum inflammation, bleeding, diminished periodontal tissue resistance to probing, gingival attachment loss, and alveolar bone recession.
Conversely, aggressive or acute apical periodontitis results in a sudden onset of severe, prolonged pain and may lead to a dental emergency. Its rapid progression, with bacteria directly damaging the periodontal tissues, causing early bone loss and tooth loosening. Chronic periodontitis can impact several teeth, while aggressive periodontitis usually focuses on a single tooth.
Researchers note that apical periodontitis is “a major public health issue that is under-recognised in many countries”; in France, for instance, two-thirds of examined patients have at least one case of apical periodontitis, often without their knowledge, with the prevalence soaring with age.
Treatment
Urgent intervention is vital for aggressive apical periodontitis. The approach to chronic periodontitis is the same but typically demands more time for detection and treatment, particularly if it affects multiple teeth.
Treatment, judged by the diagnosis, might involve cleaning the asymptomatic tooth from within under local anaesthesia and navigating the root canals. However, healing is not always guaranteed, especially when the practitioner encounters a curved root—common with molars—and cannot thoroughly clean and seal the canal’s end. Tooth extraction may then be necessary.

For a more profound periodontal impact, a dental surgeon may conduct access surgery, incising the gum to reach the infected spot, simplifying the cleaning process. With the presence of a granuloma or apical cyst, the bone must be treated and the root canal filled. Sutures get removed 10 to 15 days post-surgery. Follow-up periapical X-rays monitor the treatment’s success: if the infection resolves and the tooth is saved, good; but if not, extraction may be inevitable. Afterwards, a bone graft might be recommended to offset the periodontal bone loss, and a dental implant prosthesis could be necessary to replace the tooth, preserving the bone and ensuring continued functionality and dental health.

After treatment, localised pain may occur as the tooth nerve readjusts. If discomfort lingers, a follow-up appointment and potentially a tooth extraction should be considered.
Early Periodontitis: A Youthful Predicament
Early-onset periodontitis predominantly strikes young individuals aged 11 to 30, with girls being more commonly affected. This type of periodontitis generally manifests with mild and less obvious gum inflammation, tooth migration, bone damage, scant tartar and dental biofilm, alongside a robust level of subgingival bacterial flora. Notable indicators are lesions around the permanent molars and loss of gingival attachment for the incisors.
Treatment
A comprehensive periodontal assessment can pinpoint both the signs of periodontitis and its exacerbating factors. Through microbiological analysis, dentists can better identify the bacteria responsible for periodontitis, aiding in preventing or halting the disease’s advancement.
Addressing early periodontitis typically involves deep cleaning and root surfacing, encompassing scaling, teeth polishing, and root planing. Ultrasound technologies now enhance traditional methods for eliminating tartar accumulations. If a gum infection is present, a prescription for medication might be necessary, supplemented by a suitable antiseptic mouthwash like chlorhexidine. As a steadfast rule, diligent and frequent dental hygiene practices, including using interdental brushes, are highly recommended. Furthermore, probiotics might be introduced to restore the natural biofilm, providing protection to the teeth and gums.

Orthodontics: A Valued Ally in Combatting Periodontitis
A wealth of research supports the notion that orthodontic treatment can markedly improve periodontal health when conducted alongside proper inflammation management, suitable orthodontic force application, and impeccable oral hygiene.
The synergy between orthodontics and periodontics offers a dual benefit for dental health, enhancing the teeth’ appearance and structural wellness over the long term. With the surging interest in cosmetic dental enhancements, orthodontic solutions such as braces, veneers, crowns, as well as dental implants and prosthetics for tooth replacement, have emerged to rescue smiles marred by tooth displacement due to periodontal disease. Teeth reshaping is recommended by professionals to either address or fend off periodontitis.

Beyond improving smiles, orthodontic realignment impacts overall oral health. Properly aligned teeth reduce crowding, correct malocclusions, and balance dental arches, all of which simplify oral hygiene—a foundational element in preserving periodontal health. Research also demonstrates that the absence of orthodontic treatment may precipitate the emergence or exacerbation of periodontal conditions. Conversely, adults with misaligned teeth yet no periodontal issues often owe their good fortune to stringent dental hygiene. It is thus clear that periodontal inflammation is a prerequisite for ensuing damage.
Periodontal surgery and meticulous tooth brushing can diminish inflammation, fostering the regrowth of cementum, ligament, and bone when aligned with orthodontic measures. However, the success of these interventions is questionable without good dental hygiene, a point particularly noted in teenagers, who might neglect their oral and overall cleanliness.

Orthodontic Intervention Phases for Periodontitis
Treating periodontitis with orthodontics involves multiple steps:
- Bonding the back teeth and installing palatal arches;
- Employing back implants as supports for prosthetics;
- Temporary mini-screws are introduced to bolster the orthodontic treatment’s anchor points.
This approach not only halts the progression of periodontal diseases but can also repair and regenerate the damaged tissues, leading to sustained clinical stability. Achieving this hinges on curbing inflammation by diminishing the subgingival pathogenic load through either surgical or non-surgical means, informed by the condition’s location, the seriousness of the damage, and the patient’s dental structure. Nonetheless, administering antiseptics or antibiotics is generally reserved for more aggressive forms of periodontitis or particularly virulent bacterial infections.

Is Dental Tourism a Viable Option for Treating Periodontitis?
In response to the high costs of dental care, protracted wait times for treatment, and lack of sufficient insurance coverage in certain areas, patients increasingly turn to dental tourism for relief—and periodontal disease treatments are frequently sought after. Procedures like periodontal surgery, dental implants, prostheses, and veneers significantly combat the condition.

When periodontal disease triggers ongoing or acute pain, the first solution dental professionals offer may not always be the priciest option. However, for extensive treatment of the periodontal area impacted by one or more damaged or absent teeth or for realigning teeth with veneers that harbour bacteria, seeking ortho-periodontal treatments abroad can be a cost-effective strategy. Turkey, particularly Istanbul and Antalya, has become a hotspot for global medical tourism.

These destinations boast remarkably lower treatment costs without additional fees, offering dental rates that are 2 to 3 times less than those in France.

Appointments are typically available on short notice, and treatments can often be completed in a matter of days—all without compromising care quality, as most clinics have dentists and periodontologists well-equipped with the latest medical technology. Nonetheless, choosing a specialised agency offering all legal protections and assuring post-operative care is crucial to sidestep potential surprises.

Every year, thousands of international patients visit Turkey for dental and periodontal treatments, lured by enticing all-inclusive travel and treatment packages, with many reporting high satisfaction levels post-procedure.
12060 vues
0 commentaires
0






Il n'y a pas de commentaires pour le moment.